Endoscopic Vaginal Hysterectomy
An endoscopic vaginal hysterectomy (EVH) is a minimally invasive surgical procedure used to remove the uterus through the vaginal canal, assisted by the use of endoscopic instruments. This technique allows for the removal of the uterus without the need for an abdominal incision.
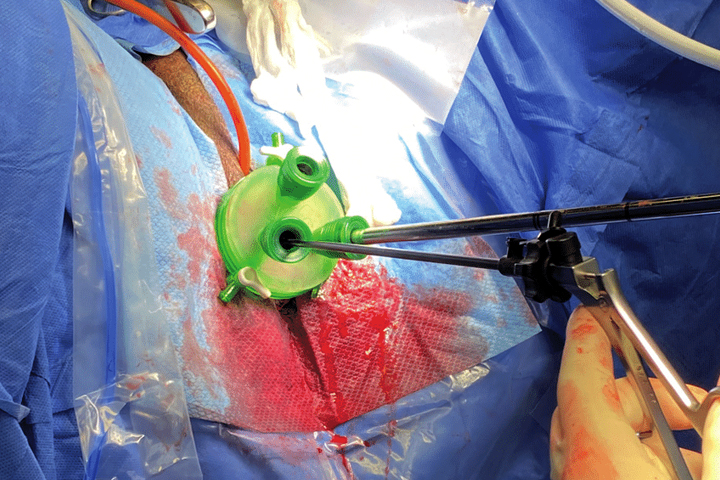
During an endoscopic vaginal hysterectomy, a laparoscope (a thin, lighted tube with a camera) is inserted through a small incision made near the navel or just above the pubic hairline. The laparoscope provides a clear view of the pelvic organs and allows the surgeon to visualize the uterus, fallopian tubes, and ovaries.
The surgical steps involved in an endoscopic vaginal hysterectomy are as follows:
- Laparoscopic Evaluation: The surgeon begins by inspecting the pelvic organs, checking for any abnormalities and ensuring that the uterus is suitable for vaginal removal.
- Detachment of the Uterus: The ligaments and tissues supporting the uterus are carefully dissected and detached from the surrounding structures, allowing the uterus to be freed from its attachments.
- Vaginal Removal: Once the uterus is detached, it is removed through the vaginal canal without the need for an abdominal incision. This is typically the primary difference between an endoscopic vaginal hysterectomy and a traditional vaginal hysterectomy.
- Closure: After the uterus is removed, any necessary repairs or closure of the vaginal cuff (the upper part of the vagina where the uterus was attached) may be performed to prevent complications and promote healing.
Endoscopic vaginal hysterectomy offers several advantages over traditional open abdominal hysterectomy, including:
- Smaller incisions: The incisions made for the laparoscope and any vaginal incisions are much smaller than those in open surgery, leading to reduced scarring and potentially faster healing.
- Shorter hospital stay: Patients typically have a shorter hospital stay compared to open surgery, allowing for a quicker recovery.
- Reduced postoperative pain: The smaller incisions and minimally invasive nature of the procedure can result in less postoperative pain.
- Faster recovery: Patients may experience a faster overall recovery and return to normal activities more quickly compared to open surgery.
- Lower risk of infection: Minimally invasive surgery generally carries a lower risk of surgical site infections compared to open surgery.
However, not all women are candidates for endoscopic vaginal hysterectomy. The suitability of this procedure depends on factors such as the size and position of the uterus, previous pelvic surgeries, and the presence of other pelvic conditions or adhesions.
As with any surgical procedure, endoscopic vaginal hysterectomy does carry some risks, including bleeding, infection, injury to surrounding structures, and the possibility of conversion to open surgery if complications arise during the procedure.
If you are considering a hysterectomy or have been advised to undergo the procedure, it's essential to discuss the available surgical options with your gynecologist to determine the most appropriate approach based on your individual medical history and condition.